The imaging facilities comprises two 3T Siemens MRI systems, one Siemens 7T system and a GE Signa PET/MR scanner. One of the Siemens MRI systems, originally installed as a TIM Trio in 2006, is currently being upgraded to a state of the art Prisma system. The centre's second MRI system was acquired as a 3T Verio system, and predominantly funded by and intended for metabolic studies in collaboration with the Institute of Metabolic Science. It has recently been refurbished as a next generation SkyraFit system and is located in the WBIC Annex, a short walk from the main WBIC building.
This wide-bore MRI scanner was originally installed in 2008 for use as a spectroscopy system. Magnetic resonance spectroscopy is an important technology in the context of metabolism and enables non-invasive measurement of biochemical intermediates and metabolic pathway activity in tissues. It has significantly advanced knowledge of both normal physiology and pathogenic mechanisms in metabolic disorders including diabetes and insulin resistance. Metabolic programs of research in Cambridge (led by Professors Chatterjee, O’Rahilly and Dunger) include the genetics of obesity and severe insulin resistance, population studies in diabetes & obesity, childhood insulin resistance, metabolic complications of critical illness, nuclear hormone receptor disorders & metabolic storage diseases. Access to a dedicated scanner wilth 1H, 31P and 13C-MRS capabilities, enabling measurement of hepatic or myocellular lipid, mitochondrial bioenergetics or activity of glucose and lipid metabolic pathways, is significantly augmenting these research programs with the potential to elucidate pathogenic mechanisms and also provide endpoints in trials of therapeutic, dietary or lifestyle intervention.
Brain Injury
The centre provides support for much of the functional imaging research in the psychology department of the University, but it is its proximity to the neuro-critical care ward that provides the primary research focus led by Professor David Menon. In the UK, head injury affects 0.5-1 million people annually, with approximately 150,000 hospital admissions, and 3,500 admissions to intensive care units. Traumatic Brain Injury (TBI) is amongst the most important causes of death in young adults, and the overall mortality for severe TBI is greater than 50%. TBI consumes one million acute hospital bed-days, and over 15,000 intensive care bed-days annually. Patients who do survive experience an enormous burden of physical disability, neurocognitive deficits, and neuropsychiatric sequelae. The cost of acute care in intensive care units is about £0.25 billion, and the NHS spends over £1 billion on overall hospital care of patients with TBI. These figures represent just the tip of the iceberg: the costs of rehabilitation and community care are difficult to estimate, but probably total many multiples of this figure.
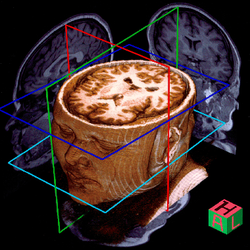
Suitable research subjects are recruited from the wards and scanned acutely as soon as possible after injury. As well as structural scans, more novel imaging protocols such as multi-direction diffusion weighted images and proton spectroscopy data are also employed. The image processing algorithms for such techniques are always evolving and the physics team at the WBIC, led by Dr Adrian Carpenter, have been active in optimising both the acquisition and analysis methodology. For example, diffusion weighted analyses have been used to demonstrate subtle changes in the organisation of the neuronal pathways in the frontal lobes. Aided by its unusual location adjacent to the ward, the WBIC is able to fulfil its original raison d’etre: “Sick patients cannot go to the scanner; the scanner must come to the patient.”
Collaboration
It is not only the acutely injured patients who are a focus for the research. There is a high profile research programme into better understanding the condition of patients with impaired consciousness. This broad categorisation encompasses conditions such as coma, vegetative state and locked in syndrome which may appear similar clinically but entail very different outcomes and treatments. A diagnosis critically depends not upon whether a patient is aware of themselves or their environment, but rather whether they retain the ability to demonstrate awareness through movement or speech (the only means a person can signal they are aware and conscious). Clinical audits have suggested up to 43% of patients are misdiagnosed largely due to this requirement. We are exploring new technologies to improve the accuracy of assessment and facilitate interventions to improve recovery and quality of life. It is estimated that between 12 and 15 persons per million might be in a vegetative state up to 6 months post injury, with three times this figure in a minimally conscious state. Based on average high dependency care costs, for patients in a vegetative state alone, this is a weekly cost to the NHS of £3.4 million.
Dr's Martin Coleman and Adrian Owen demonstrated in a seminal Science paper that fMRI paradigms are capable of detecting awareness in patients behaviourally meeting the criteria defining the vegetative state. Clinically the patient investigated demonstrated no evidence of awareness or purposeful response to command when she was asked to move or speak. However, when asked to perform several mental imagery tasks during fMRI the responses obtained were indistinguishable from healthy volunteers performing the same task. Hence, despite negative behavioural markers, it was possible to detect awareness without requiring the patient to move or speak.
With such a strong community of researchers based locally, and state of the art facilities, the WBIC is an extraordinarily well placed organisation to perform research into acute injury at the same time as explore new directions in metabolic medicine.
